If you’ve been diagnosed with keratoconus, treatment depends on how fast the condition is progressing. The top eye specialists at Austin Eye discuss when corneal crosslinking is recommended for patients with keratoconus.
Keratoconus
The cornea is the transparent part of the front of the eye. Covering both the iris and pupil, the cornea’s function is to allow light to enter. The cornea bends that light onto the lens, followed by the lens’ refocusing of the light onto the retina. The retina, in the back of the eye, starts the conversion of light into vision.
In keratoconus, the cornea starts thinning. Eventually, the cornea bulges outward into a cone-like shape. Unlike many eye conditions, keratoconus often affects young people, beginning as early as 10. Keratoconus usually involves both eyes.
Symptoms of keratoconus include:
- Blurred vision
- Increased sensitivity to light and glare
- Frequent need for new eyeglass prescriptions
- Sudden vision worsening
Risk factors include a family history of the disease. Certain conditions increase the risk of developing keratoconus. These include:
- Asthma
- Down syndrome
- Ehlers-Danlos syndrome
- Retinitis pigmentosa
Mild To Moderate Keratoconus Treatment
Mild to moderate cases of keratoconus are generally treated with eyeglasses or contact lenses. If your cornea stabilizes, this is potentially the only treatment necessary.
Corneal Crosslinking
For those whose keratoconus is progressing, corneal crosslinking can help stop vision loss. It is a minimally invasive procedure to boost corneal strength. Ultraviolet light combined with eye drops strengthens the cornea’s collagen fibers. Collagen, a protein that is one of the body’s building blocks, holds the cornea together.
Although available in Europe for many years, corneal crosslinking is relatively new in the United States.
Keep in mind that corneal crosslinking cannot reverse the disease or improve your vision. The good news is that the procedure can prevent the need for more invasive treatment, such as corneal transplant surgery, down the road.
Corneal Crosslinking Procedure
If you wear hard contact lenses, your eye doctor will have you stop wearing them several weeks before your scheduled procedure.
Corneal crosslinking consists of the doctor removing the epithelium, the cornea’s thin outer layer. This removal permits medication to go deeper into the cornea. Next, the doctor applies Vitamin B2 eye drops into the eyes. A specific type of UV light is then shone onto the cornea for approximately 30 minutes.
The actual procedure takes up to 90 minutes. Patients receive mild sedation and are awake the entire time.
Corneal Crosslinking Recovery
Some patients experience pain after corneal crosslinking. There is often a gritty feeling in the eyes. Over-the-counter pain medications should prove sufficient to control discomfort, but your eye doctor may prescribe stronger painkillers if OTC products are not sufficient.
Avoid rubbing your eyes for a few weeks after corneal crosslinking. Your eye doctor will let you know when you can resume wearing contact lenses. For most patients, that’s at least a month post-procedure.
There is no change in the appearance of your eyes after corneal crosslinking.
Contact Us
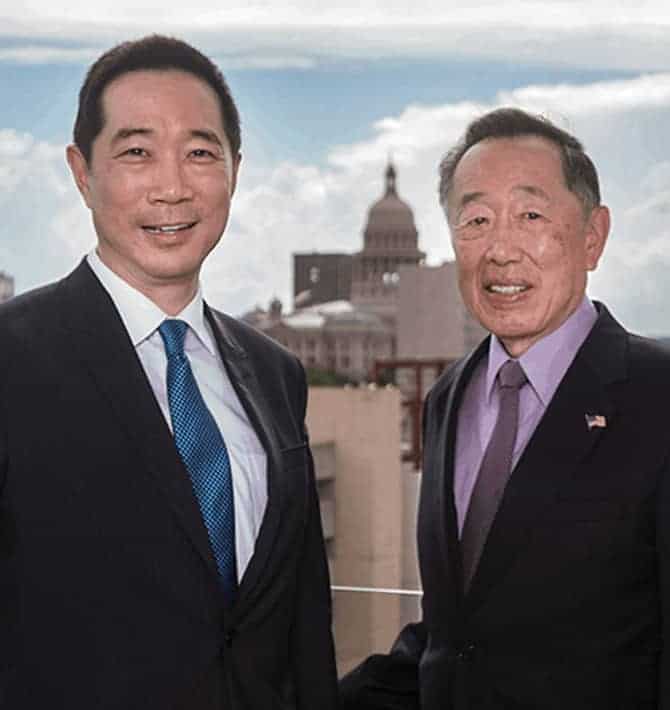
If you have been diagnosed with keratoconus or are experiencing symptoms of the disease, contact the dedicated eye care specialists at Austin Eye to schedule a consultation.