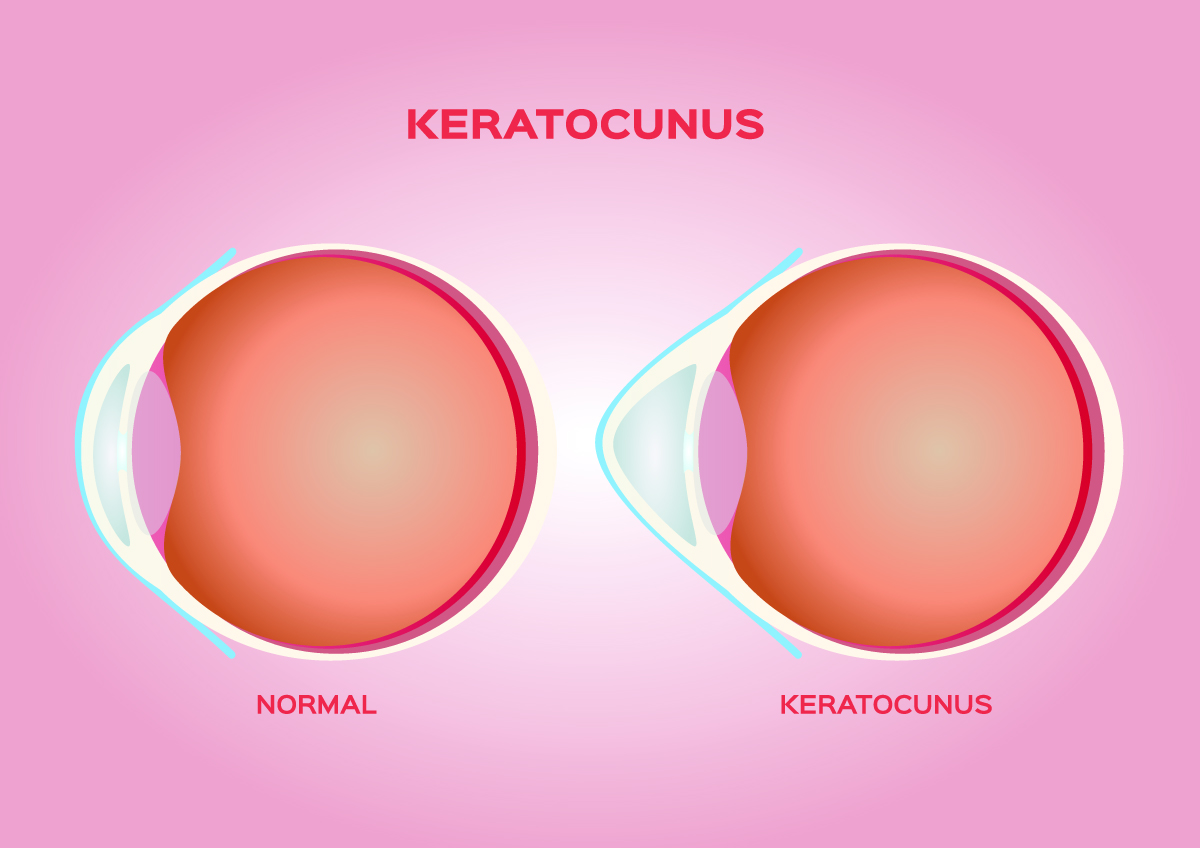
Keratoconus is a progressive condition that weakens the cornea, causing it to thin and bulge out. Good vision relies on the dome-shaped cornea to refract light onto the retina, but keratoconus distorts the corneal shape, which leads to blurry eyesight, glare and light sensitivity. Our ophthalmologists offer corneal collagen cross-linking to slow the progression of keratoconus and provide long-term improvement that reduces the need for a corneal transplant for many patients.
Early keratoconus can be managed with eyeglasses and soft contact lenses, but the condition worsens for around 20 years, causing frequent vision changes through your 30s and 40s. Corneal collagen cross-linking, especially performed early on, prevents many patients from needing a corneal transplant, and most patients have minimal vision changes 10 years after the procedure.
What is Corneal Collagen Cross-Linking?
Corneal cross-linking works by strengthening collagen fibers in the eye that anchor the cornea and help maintain a normal corneal shape. The procedure prevents or stalls further bulging and improves the focusing ability of the cornea for better eyesight. Riboflavin (Vitamin B2) drops are administered in the eye and then a UV light activates the eye drops to increase the collagen “cross-links” in the affected cornea.
Our Austin eye surgeons perform corneal cross-linking in two ways. The first method removes the epithelium, or thin surface layer of the cornea, so that the riboflavin drops will be able to penetrate the cornea quickly. Our other technique leaves the epithelium intact, though it takes longer for the riboflavin drops to soak into the cornea.
Patients often require glasses or contact lenses after corneal cross-linking, but the lenses will be more comfortable.
What the Research Says About Keratoconus and Corneal Cross-Linking
This keratoconus treatment was FDA-approved in 2016 after three phase-three clinical trials showed successful results. A 10-year follow-up with some of these patients found their vision remained stable a decade after corneal collagen cross-linking with no significant side effects or safety issues.
The long-term stability of this treatment not only improves quality of life but lowers the cost of care. An economic analysis of corneal cross-linking for keratoconus patients in 2021 found that patients spent 27.9 fewer years in the advanced stages of keratoconus and were less likely to need penetrating keratoplasty, a type of cornea transplant. The researchers’ model suggested a cost savings of $43,759 per patient. That estimate is higher when the disease is treated with the procedure early on or when the patient is younger because it extends their ability to work, reduces medical expenses and enhances quality of life by saving more of the patient’s vision.
If you have been diagnosed with keratoconus or are experiencing symptoms of this condition, contact Austin Eye to schedule a comprehensive eye exam with our board-certified ophthalmologists. Call our Austin, Texas office at (512) 250-2020 or fill out our online contact form.